Services Offered
Click on one of our services below to see how we can help.
Like To Book One Of Our Services
Contact us today for advice and a discussion on what is the best route forward for your condition.
Like To Discuss What Service You Need
If so, get in touch with us today for a consultation. We will assess if we have a service for your condition.
List Of Services
Regenerative Medicine
Regenerative medicine is still deemed experimental in the United States. It is not covered by insurance or medicare. However, the results are so impressive that people like Stephen Curry and Kobe Bryant are traveling overseas to get it.
The human body is in a constant state of degradation and repair. If we sustain an injury, tissue factors are released and this leads to a cascade of chemical signals that starts the repair process. This is known as “inflammation”. These signals call small cellular workers to the site of injury that clean up the debris and signal the surrounding area to lay down new tissue.
However, as we age that balance gets tilted towards more degeneration, and less regeneration. Due to a variety of genetic, environmental, and other factors, the inflammation is there but the process of repair is sluggish. Injury occurs and the site doesn’t completely heal, leading to scar tissue, poor blood flow, and chronic pain.
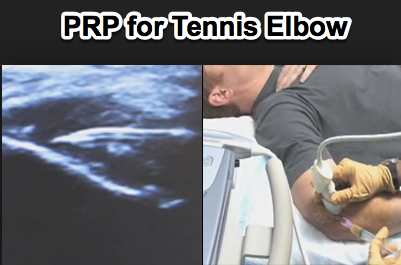
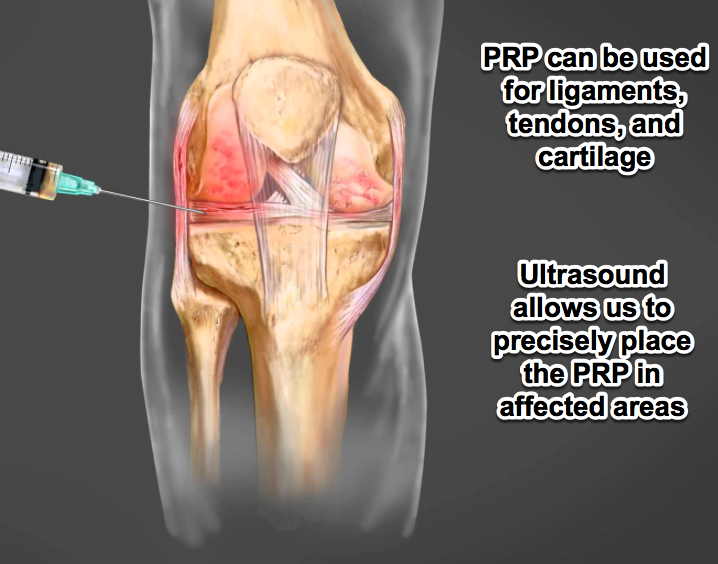
Platelets are a key cellular component to this process. When injury occurs, they release a myriad of chemical growth factors and signals that starts the process. We can now use this to our advantage. We can draw blood from your body and spin it down in a centrifuge. This separates the sample into layers of red blood cells, platelet poor plasma, and platelet rich plasma. It is the platelet rich plasma (PRP) that is drawn off and reinjected into your site of chronic injury.
This supraphysiologic concentrate has over thirty growth factors and signaling molecules. And best of all, it’s your tissue. There’s no chance of allergic reaction or rejection. Complications are incredibly low; much lower than putting medications and other foreign substances into your body.
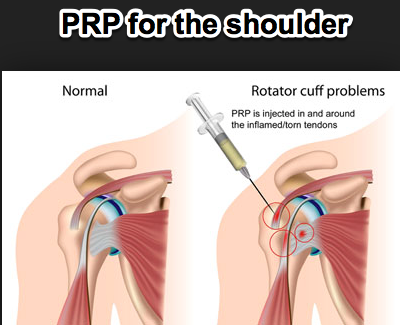
This therapy is extremely effective for soft tissue injury like tendons and muscles. Tennis elbow, rotator cuff tendinits, bursitis of the hip, and plantar fasciits all respond very well to this therapy. The next most common area is injection into the knee, hip, and shoulder to treat cartilage injuries. And finally, early data is showing promising results by injecting it into the discs and facet joints to treat chronic back pain and avoid surgery.
The illustrations below demonstrate how we extract the PRP and areas we can treat.
As I stated in the beginning, this is considered experimental and is not covered by insurance or medicare. It is paid entirely by the patient. However, many patients have failed all other options and like the idea of using their own tissue factors to heal their body and avoid medications or surgery. I have used it on myself multiple times and I have been extremely happy.
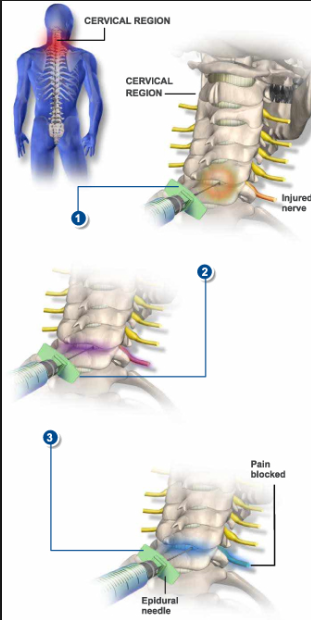
Cervical Epidural Steroid injections
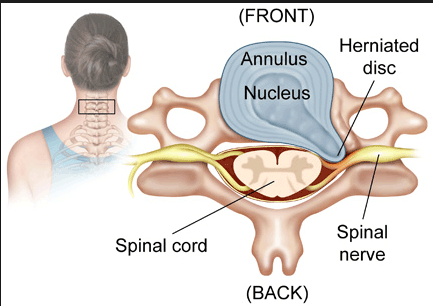
Nerves in the neck can be pinched for a variety of reasons. Bulging discs, enlarging facet joint, and degeneratve changes can all lead to nerve impingement. The diagram below illustrates what happens.
When nerves are compressed they react with swelling and inflammation, only worsening the impingement. A vicious cycle of pain, swelling, inflammation, and further impingement can occur. Epidural steroid injections act to break that cycle by bathing the affected in steroid, an anti inflammatory medication. Patients will often require a series of injections to achieve full relief. Patient should also include medications, physical therapy, and massage.
You will receive an IV for this procedure and mild sedation. It is important that you are still conscious for this procedure, as bumping of the nerve can occur and general anesthesia would mask this complication. We will gently talk you through the procedure and it is well tolerated. Patients should expect relief in the first three days, as it takes some time for the anti-inflammatory effect to take place.
Medial Branch block: Cervical, Thoracic, and Lumbar
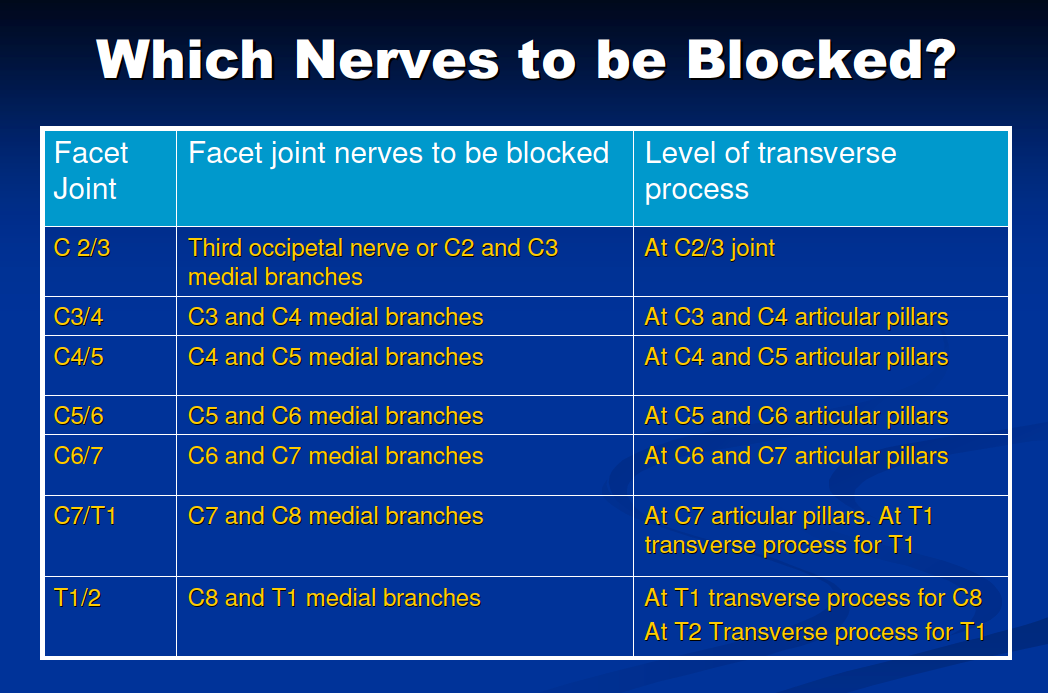
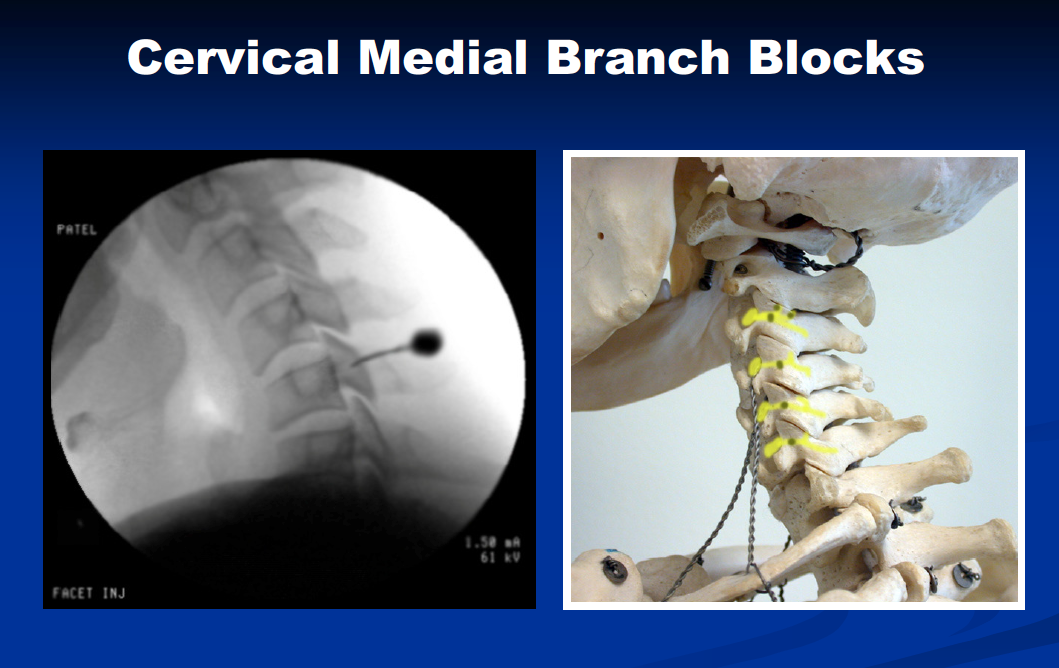
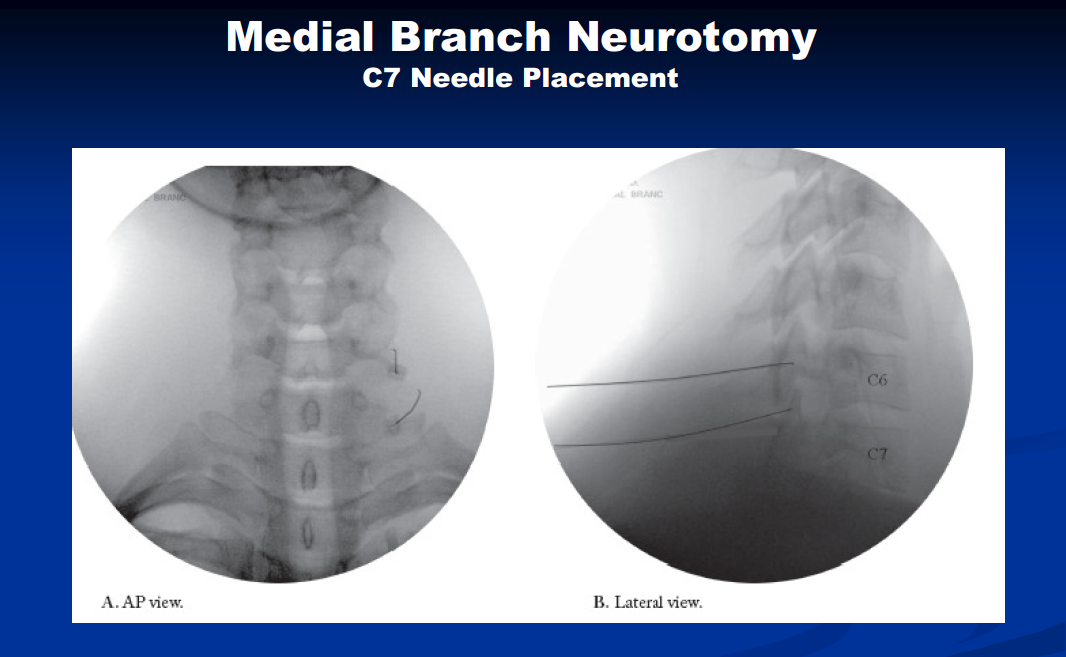
Joints of the spine are called facet joints. The facets vary depending on the level in the spine. However, the medial branch innervates all facets. The diagrams below show you what they look like and the table illustrates which level we go after based on the level that is diseased.
Facets are one of the most common sources of pain. Placing local anesthetic on the medial branch allows us to diagnose that your pain is coming from these joints. Unfortunately, imaging alone cannot answer this question. That’s why these are called “diagnostic blocks”. They are used to diagnose where your pain is coming from. The bottom diagram illustrates proper needle placement.
Studies show that there can be a high rate of placebo with only one block; so performing an initial and confirmatory block is necessary. We will assess your pain before and after the procedure. A significant reduction in your pain, which matches the duration of the local anesthetic, confirms that this is the source of your pain. We can now proceed to the therapeutic treatment for facet disease, a radiofrequency ablation.
Radiofrequency Ablation: Cervical, Thoracic, and Lumbar.
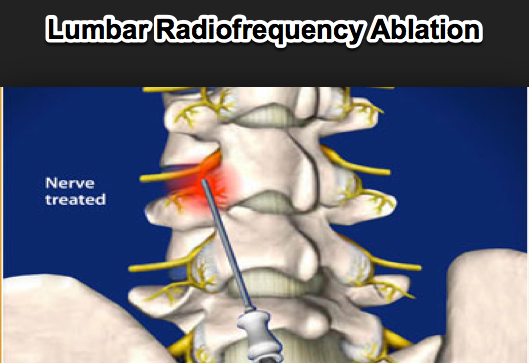
Radiofrequency ablation is a minimally invasive technique that can have dramatic results in the right patient. If you have undergone successful initial and confirmatory medial branch blocks for facet disease, than you are a candidate for Radiofrequency ablation.
You will have an IV started and mild sedation is given. The area is sterilely prepped and we gently place a radiofrequency probe on the bony area of the facet, which contains the medial branch. We then do sensory and motor testing by attaching the probe to a radiofrequency generator. Sensory testing will cause you to feel the same pain you normally do by stimulating the nerve. Motor testing will cause the small muscles on the joint to gently move the needle up and down. We should not see your arm or leg move. This would indicate misplacement of the needle and proper adjustments will take place. Needle placement is also confirmed with a live X ray machine throughout the procedure.
Local anesthetic is given through the probe and a thermal lesion the size of a q-tip occurs over ninety seconds. It should not be painful and we will be monitoring your throughout the procedure. Steroid is given in the needle at the end to minimize inflammation and pain after the procedure.
Patients will notice some soreness for the first couple of days since we have caused a thermal lesion. Rarely patients experience a neuritis, or irritation of the nerve that can last up to a week. Most patients tolerate the procedure quite well.
As with other tissue in the body, these nerves will regenerate.
Patients can expect 6 months to 6 years of long-term relief depending on the severity of your condition.
This procedure has revolutionized spine care and can provide lasting relief without the need for surgery.
Lumbar Transforaminal Epidural Steroid Injections. (TESI)
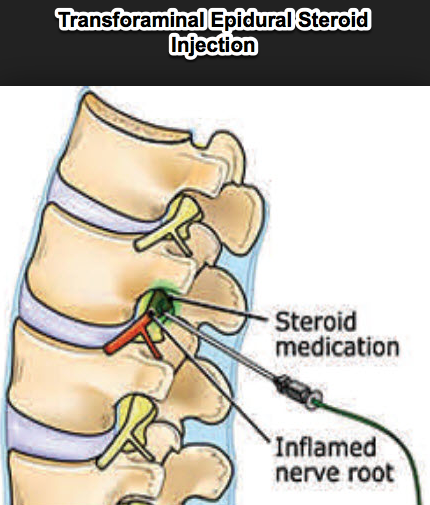
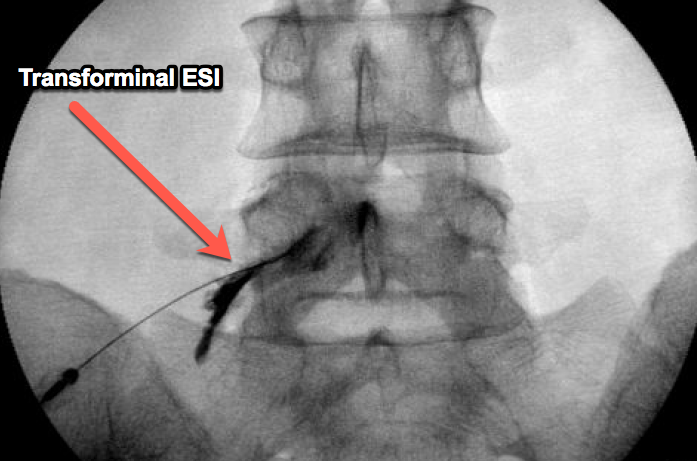
Lumbar TESI injections are a unique injection that places epidural steroid in the neural foramen, the area of the spine where the nerve root exits. This is the most common area of nerve impingement, often from a disc or enlarged facet. By placing the medication right at the site of irritation we maximize your chances of success.
An IV is started and sedation is given. You will not be under general anesthesia. Pathology in the spine can cause distortions that push the nerve into areas that it normally does not reside. As we approach the foramen, we will cautiously advance the needle and ask for any signs of bumping the nerve. You may feel a mild parasthesia into your leg, which will allow us to adjust the needle accordingly. Practitioners putting patients under general anesthesia place you at risk of injecting into the nerve, which could have long lasting consequences. Once the area is localized, dye is injected under live X ray to confirm proper needle placement. Anti-inflammatory steroid is then injected and the procedure is complete.
Patients should see a positive effect in the first three days after the procedure as the medication takes effect. Often a series of injections is needed to undo the cycle of compression, pain, and inflammation of the nerve.
Epidural steroid injections have provided lasting relief to many of our patients, especially when combined with core strengthening, traction, and intermittent bracing.
Kyphoplasty
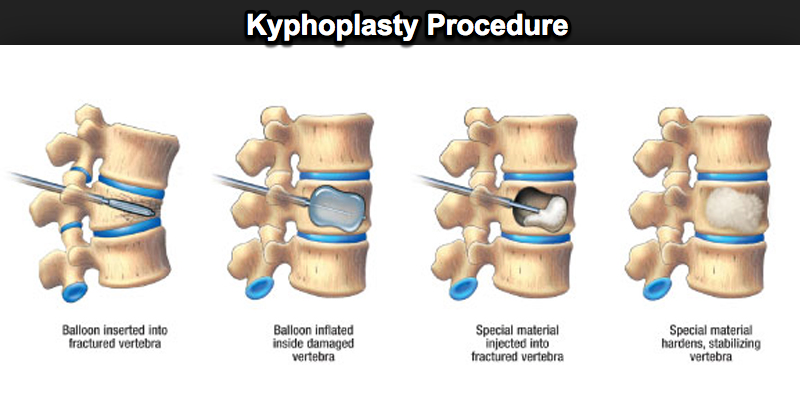
Kyphoplasty is a minimally invasive procedure that has helped many Americans who suffer compression fractures. The large amount of patients with osteoporosis makes this procedure a valuable tool in their treatment.
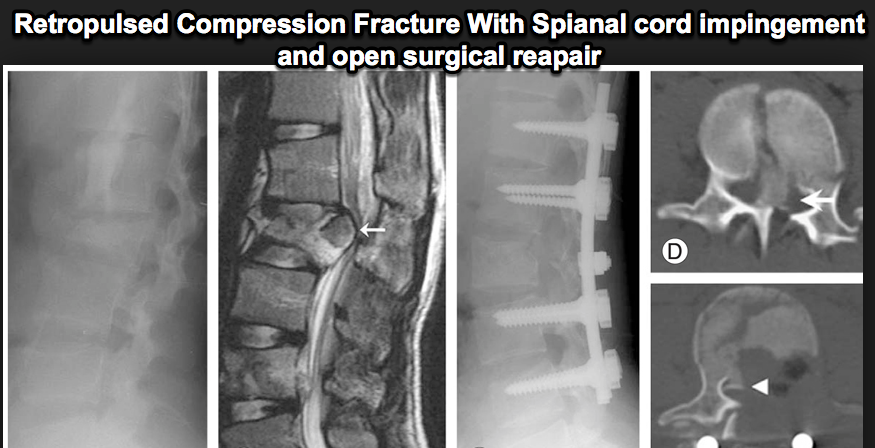
Compression fractures tend to do two things: cause pain and progress. The ongoing pain can prevent them from walking and breathing properly, predisposing them to lung dysfunction and clots. The settling of the fracture leads to a postural deformity known as kyphosis, a c shaped abnormality of the spine seen in many of our older patients. And lastly, this progression can cause retro-pulsion of bone fragments back into the spinal cord. See the bottom two diagrams showing a compression fracture as well as what retro-pulsion looks like on MRI.
Kyphoplasty achieves three primary goals. If caught early, it can reestablish the height of the vertebral body back to its normal configuration, preventing the postural deformity. It fixes the pain, as the fractured bone no longer moves around irritating the fibrous lining of the backbone. And finally, it stabilizes the fracture preventing progression and retro-pulsion into the spinal cord.
An IV will be started and sedation given. A live x ray will be used to identify the area in both the straight on view and lateral view. Skin marks will be placed on your skin and local anesthetic will numb the skin, subcutaneous tissue and periosteum over the bone. A device called a trochar is advanced carefully into the vertebral body through a structure called the pedicle. A balloon is then inflated under live X ray to assure proper placement and reestablishment of height. Depending on the location of the balloon, this may be repeated on the other side. This balloon creates a void in the bone, and cement is then injected into that void to stabilize the fracture. Careful attention is focused on assuring that the cement stays in the anterior two thirds of the vertebral body and that it crosses the mid portion of the vertebral body. The cement is dry within 10 minutes and the procedure is complete.
Patients can resume regular activities within a day. You may have some mild soreness from passing the trochar in soft tissue.
Cement traveling along a fracture line backwards into the canal is always a risk. However, if you take the time to place two introducers, create two voids, and proceed carefully your risk is greatly reduced.
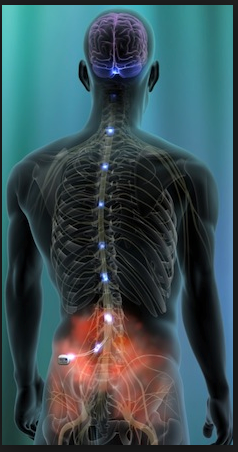
Neuromodulation: Spinal Cord Stimulator/Peripheral Nerve Stimulator
Neuromodulation is an advanced pain management technique used for intractable neuropathic pain. Conditions that can be treated with this include diabetic neuropathy, chronic radiculopathy, failed back surgery syndrome, reflex sympathetic dystrophy, and phantom limb pain to name a few.
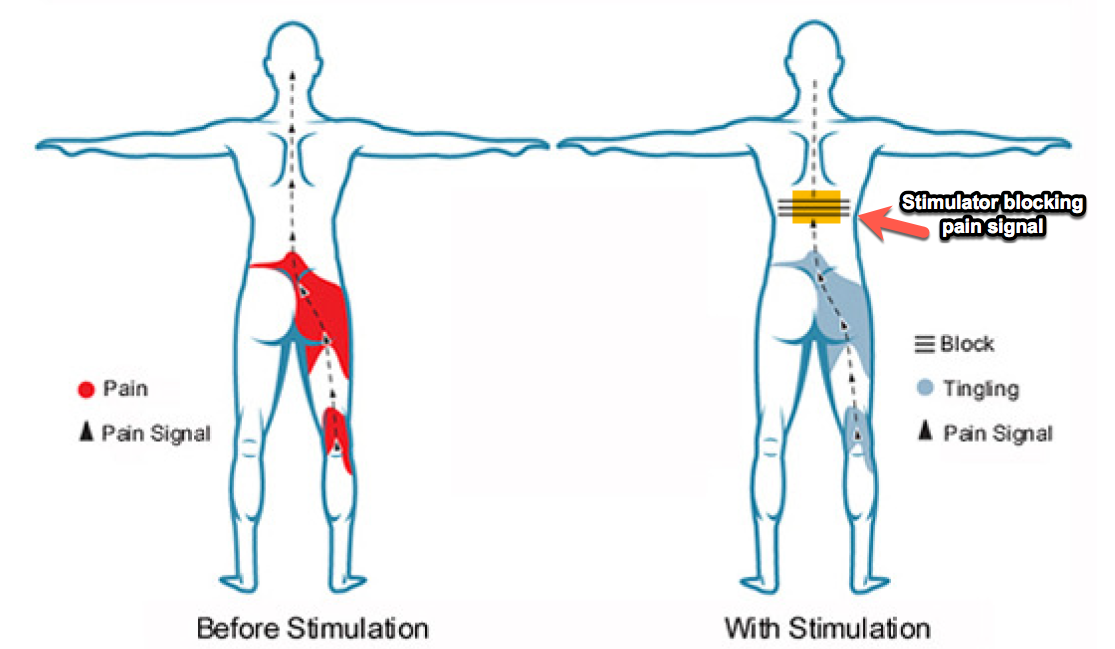
It works by what is known as the “gate theory”. Special leads are placed in the epidural space and it is attached to a generator. Low voltage impulses are generated and transmitted superficially in an area of the spinal cord called the dorsal column. The patient now feels a tingling sensation instead of pain, and the electrical stimulation is acting to “close the gate” such that pain signals coming from below can’t reach the brain since the stimulator is occupying the pain tract. Another analogy would be a car trying to enter the freeway in a traffic jam. You (the pain signal) can’t get on the freeway because of the continual stream of cars passing by (the stimulator signal). Check out the top diagram for a schematic of this .
Since this is a permanent implant patients must undergo a trial to be sure that this therapy is right for you. During the trial, an IV is placed and the stimulator leads are advanced under live fluoroscopy to the appropriate level in the spinal cord. The leads are attached and you are asked if you feel the stimulation and if it’s covering the area of your pain. Adjustments are made to the generator and lead position until proper coverage is achieved. It is firmly taped and the procedure is complete.
The manufacturers representative will be in contact with you for five days after the procedure. After that the leads are pulled. If you had an excellent result you may be a candidate for permanent implant.
The permanent implant is the same as the trial except this time a small pocket is made under the skin, usually over the right or left hip. A battery is placed, the leads are tunneled under the skin, and the system is connected and proper functioning is tested. The small incision sites are closed and the patient is discharged the same day. The bottom diagram shows the usual battery location under on the hip in a pocket under the skin.
This technology has proven to be one of the most effective treatments for intractable neuropathic conditions such as chronic radiculapathy, failed back surgery syndrome, diabetic neuropathy, and reflex sympathetic dystrophy to name a few. Patients with medical problems who can’t have surgery but have chronically pinched nerves do very well. It can truly change the lives of patients living with these debilitating problems.
Genicular Block / Radiofrequency Ablation
This is an exciting new procedure that few clinics are offering. The genicular nerves are sensory nerves that innervate the knee. Studies have shown that they follow predictable patterns base on bony anatomy, and can be blocked or ablated depending on the need. The diagram below illustrates this.
Genicular block/Radiofrequency ablation is a great option for patients that have had a total knee replacement or are not candidates for a knee replacement. This can be due to other medical risks or personal choice to delay surgery.
An IV is started and you will be lying supine on the procedure table. The knee area is evaluated under live x ray and the area of the skin is numbed. We gently place the needle in the area of the genicular nerves and place long acting local anesthetic. If you notice a dramatic reduction in your pain after the initial and confirmatory block, than you are a candidate for radiofrequency ablation.
Patients can expect six months to six years of pain relief depending on the severity of your condition. We have seen some impressive results.
Medication Management
Proper medical management is mandatory for comprehensive pain management. We use a wide variety of non-opiate and opiate medications depending on your condition. Our approach has been constructed with the expertise of the American Society of Interventional Pain Physicians as well as other national experts.
We are careful to prescribe medications that are specific to your condition. Our goal is to maximize function. Nobody likes to take unnecessary medication and we are mindful of this in our practice. We will monitor you for side effects as well as screen you for anxiety, depression, and addiction risk. We will set SMART goals with you, specific measureable, achievable, realistic and timely goals that matter to you. We screen all of our patients with a UDS (urine drug screen). This is a standard practice that protects both you and your provider. It should be viewed as any other lab test. We are assuring that the proper medication is in your system and that you’re not on any illicit substances. Regulatory agencies are clear that using illicit drugs with opiates is not allowed. Non-opiate therapy and other interventions will still be offered and can be extremely effective depending on your condition. We will also have a medication contract with you that will explain all of this and assures that these medications are available for the people who need them.
Our goal is to maximize you function, limit side effects, and assure maximum success. The illustration below reminds us that all medications have side effects and be mindful of this when using them.
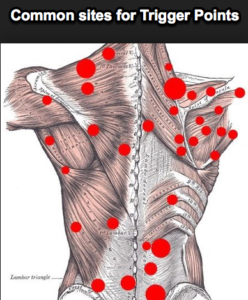
Trigger Point Injection
Trigger points are an area of muscle injury that is in continual spasm. This causes localized pain as well as referred pain. Once a trigger point is identified, we can inject it under ultrasound guidance and achieve quick relief. The area is sterilely prepped and confirmed with palpation and ultrasound. A small needle is gently advanced into the focal area of spasm and gently injected with local anesthetic and steroid, thereby breaking up the spasm allowing blood flow and healing. Patients usually feel very good the first day due to the local anesthetic. They often feel a bit sore on day two from the mild trauma of the injection. After this blood flow can reach the injured area and healing commences. The procedure is low risk and well tolerated. It requires no sedation and can be done in the office
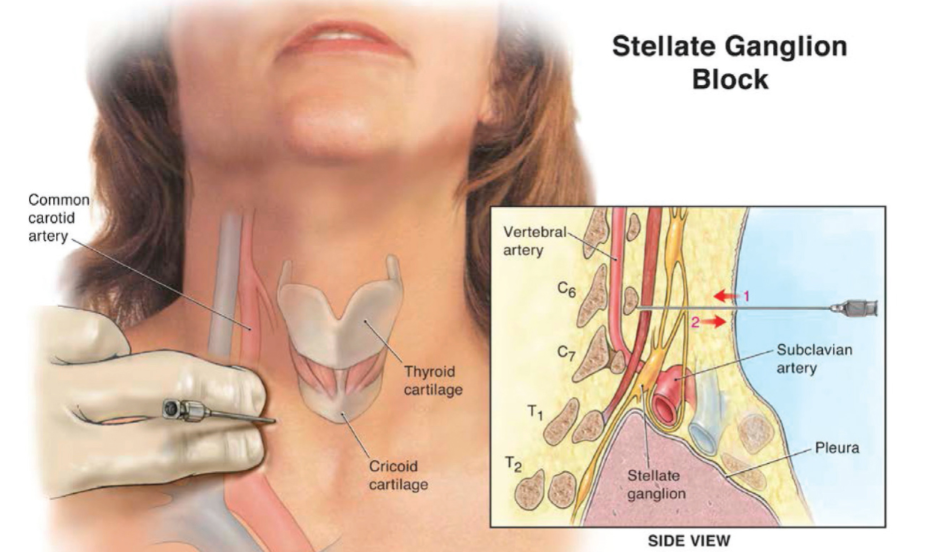
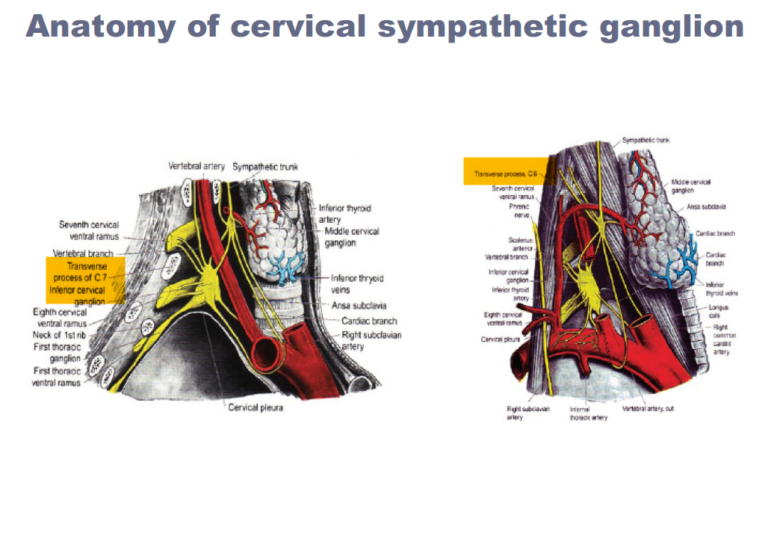
Stellate Ganglion Block
This procedure is performed on patients who have reflex sympathetic dystrophy of the upper limb. You will have an IV placed and lay supine on the table. An ultrasound will be used to identify the area and a needle is gently advanced to the target area. Under live ultrasound local anesthetic will be given to assure proper placement and a good result. After we will assess temperature differences both before and after. A positive temperature change indicates a good result.
Often patients need a series of these injections to achieve lasting results. As mentioned previously, early and aggressive intervention is key to preventing lasting disability from this condition.
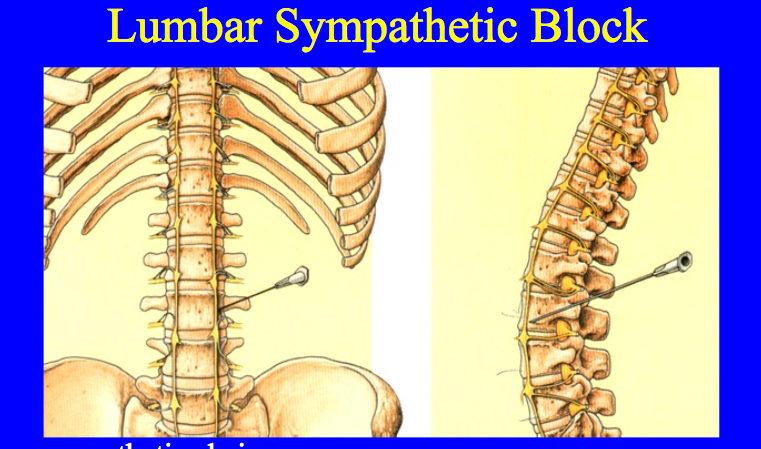
Lumbar Sympathetic Block
Patients with reflex sympathetic dystrophy of the lower limbs are candidates for this procedure. An IV will be started and you will lye face down. A live x ray will identify the proper level. A needle is gently advanced to the anterior portion of the vertebral body and dye is injected. Careful attention is paid to prevent uptake into a vessel. Once this is confirmed, local anesthetic is given and the procedure is complete. The two diagrams below show you where the sympathetic chain lyes and the dye pattern we look for during the procedure.
An elevation in temperature of the affected limb is indicative of a successful block.
Often patients need a series of these injections to achieve lasting results. Early and aggressive intervention is key to preventing lasting disability from this condition.
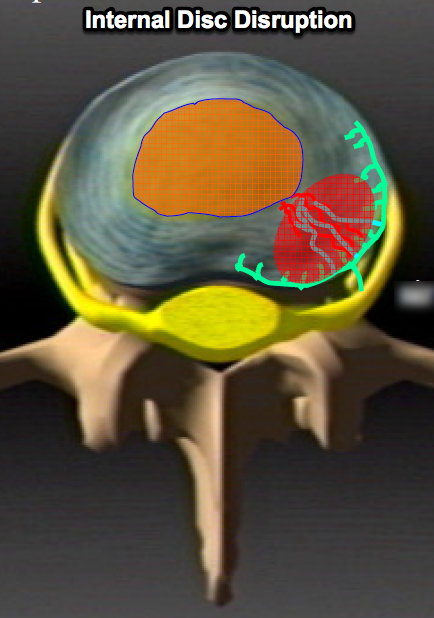
Discography
This is a procedure used to diagnose painful discs. Discs normally aren’t painful. Only the outer portion of the disc has pain fibers. As discs degenerate, the inner jelly of the disc can come in contact with the outer pain fibers causing the disc to become painful. This is known as discogenic pain. It can be very debilitating, and proper diagnosis will help guide treatment.
The top diagram shows you how a tear into the area that has pain fibers starts this condition. The X ray shows the dye patterns for a discogram, and the one below that shows the various ways a disc can tear outward and how we classify these.
Anterior Cervical Discectomy and Fusion (ACDF)
This procedure is not offered in our practice but is here for educational purposes. For patients that have a compressed nerve in the neck and have failed conservative treatment, an ACDF may be what is necessary for you.
This procedure is performed through a small incision in the front of the neck. The muscles, vessels, and esophagus are gently deflected out the way. The front surface of the spine is exposed. A microscope is used for the rest of the procedure. The disc is removed as well as any soft tissue that may be causing nerve impingement. The remaining space is measured and the appropriate spacer placed between the bones where the disc used to live. A plate is then placed across the areas of interest. X ray is used to confirm proper placement. The area is washed and the wound closed.
The most common levels are C5/6 and /or C6/7. It is rare to require more than a two level fusion.
You can expect to go home the day of surgery or after an overnight stay. The bones start to fuse together by 6 weeks and physical therapy is initiated.
Minimally Invasive Lumbar Decompression and Interbody Fusion
This technique is not offered in our practice but patients have asked me what it is.
I discussed this with Dr. George Galvan, a neurosurgical colleague of mine that specializes in this procedure. The advantages of this approach compared the traditional approach are as follows:
- This procedure can be performed thorough a 3 inch incision, often on one side only.
- It avoids the muscle stripping of the traditional approach. This leads to a reduction in pain, less blood loss, and less spasm.
- The intact muscles are left to provide additional ongoing structural support.
- Decreased risk of postoperative seroma and potentially infection.
This is more tailored to the 30 to 60 year old patient with isolated disease. If you have severe multi level stenosis than you may not be a candidate for this procedure. Your surgeon will review your images and discuss the options with you.
Posterior Lumbar Decompression and Interbody Fusion (PLIF)
While a miniminally invasive approach has its advantages, some patients have such advanced disease that they are not candidates for a minimally invasive approach. They have collapsed disc spaces, severe facet disease, soft tissue overgrowth, and profound spinal stenosis.
In this case, the posterior element of the spine has to be removed in its entirety as well as the discs between the spine bones. An interbody bone spacer is placed between the vertebral bodies to re establish the proper height and the segment is stabilized with screws and rods. The approach does result in a fair amount of blood loss due to the necessary surgical dissection. Despite the breadth of surgery entailed in this procedure, the person with profound disease will see significant improvement over the long term.
Let’s Get StarteD TODAY
Contact Us Today For A Consultation
Idaho Pain & Spine
1859 S. Topaz Way, Meridian ID 83642
(208) 672-4640
(208) 957-6300